Tuesday, December 30, 2014
Fun Video Blog Break: Tim Hawkins on Breaking Mom
I LOVE comedian Tim Hawkins. Enjoy his discussing the importance of giving moms a break.
Thursday, December 25, 2014
Video Blog Break: Imperfect Perfection
What is the value of a life? This dad teaches us a lot about it.
Sometimes our ideas of perfection get turned upside down. But if we can focus on what God might be teaching us, we can come away with a much fuller life filled with imperfection.
Merry Christmas.
Tuesday, December 23, 2014
Fun Video Blog Break: Stayin' Alive
One of my favorite videos from this year was Chattanooga Firefighters using some creative teaching in how to do proper CPR.
Great work, guys. I always love a medical lesson taught in an inventive way.
Thursday, December 18, 2014
Fun Video Blog Break: Tim Hawkins
My favorite comedian is Tim Hawkins. There're tons of videos of him on You Tube. If you need a good laugh, check out his other videos.
Tuesday, December 16, 2014
Fun Video Blog Break: Jimmy Fallon Hashtags "WorstGiftEver"
Starting off our funny blog break is Jimmy Fallon. If you're not watching the show, he does a weekly hastag. This one is #WortstGiftEver.
What was your worst Christmas gift ever?
Thursday, December 11, 2014
Author Beware: Medical Students
I've blogged here a lot about the trouble many authors have with scope of practice issues. Scope of practice is what the licensing board says you can and can't do to a patient. Every licensed healthcare professional has a defined scope of practice. For nurses, it is managed by their State Board of Nursing. For doctors, it is the Board of Healing Arts.
You can find other posts I did about scope of practice here, here and here.
I recently came across a novel written by a doctor that had an interesting medical scenario. In short, a medical student was running amok killing patients by overdosing them on potassium. Below are a few highlighted portions from the novel. I'm using asterisks instead of characters names to further disguise the story to protect the author.
This portion is written from the medical student's (the killer's) POV:
I was helping them (nurses) with their work. I've fixed IV pumps, drawn blood, placed catheters, even changed bedpans. It's got me into their good graces, and a lot of them now pretty much trust me with anything. Like giving medications.
They'd pull the IV bag from the electronic medication dispenser, log it into the system, hand it to me, and go back to doing the twenty other things they were trying to do at the same time. They never gave me or my poor little bag of potassium a second thought.
And why not? They'd seen me give IV medications to patients hundreds of times. Not one of the-- not a single one-- even bothered to check to see if the patient actually needed potassium, much less confirm that I'd actually given it."
Honestly, it's hard to know where to start with the medical inaccuracies this small piece of fiction highlights.
1. A medical student is not licensed healthcare provider. Therefore, they practice under someone else's license. They are managed by their attending physician or resident. They are not monitored by nursing. A nurse is not going to let a medical student do these things to her patient. The most a medical student does is obtain a patient history, do a physical exam, and observe procedures by other physicians. If this author had made the medical student a resident-- the scenario would be a little more plausible.
2. Every nurse is not that stupid. Sure, one nurse allowing a medical student to give her potassium I could believe. But, as in the novel, up to fifty? Remember, the nurse is likely more liable than the medical student under this circumstance. These nurses would all be fired. Nurses are not that blase about their licenses. Without one, even a license with a minor mark, and that nurse will not be working in nursing ever again. Medical students are learning. A nurse's job is to protect her patient. We don't trust medical students to be competent in what they're doing for that reason alone.
3. The author also misses another layer of protection. Medical dispensing machines are another layer of protection. Hospital medications are approved for dispensing by the hospital pharmacist. So, a pharmacist can look up a patient's lab results and check whether or not they need the potassium as well. All these medication orders on patients that don't need potassium is going to raise some serious alarms. Can you override the medication dispensing system? Yes, but you better have a good reason. Many hospitals have removed concentrated forms of IV potassium because an error could be so potentially deadly to the patient. Also, patients who receive a bolus dose of IV potassium need to be placed on an ECG tracing (or continuous heart monitoring.) In this instance, they are generally in the ICU or on telemetry and not a basic med/surg unit.
The scenario could be plausible if written another way. Overall, the author needed a seasoned ICU nurse to review the manuscript.
You can find other posts I did about scope of practice here, here and here.
I recently came across a novel written by a doctor that had an interesting medical scenario. In short, a medical student was running amok killing patients by overdosing them on potassium. Below are a few highlighted portions from the novel. I'm using asterisks instead of characters names to further disguise the story to protect the author.
This portion is written from the medical student's (the killer's) POV:
I was helping them (nurses) with their work. I've fixed IV pumps, drawn blood, placed catheters, even changed bedpans. It's got me into their good graces, and a lot of them now pretty much trust me with anything. Like giving medications.
They'd pull the IV bag from the electronic medication dispenser, log it into the system, hand it to me, and go back to doing the twenty other things they were trying to do at the same time. They never gave me or my poor little bag of potassium a second thought.
And why not? They'd seen me give IV medications to patients hundreds of times. Not one of the-- not a single one-- even bothered to check to see if the patient actually needed potassium, much less confirm that I'd actually given it."
Honestly, it's hard to know where to start with the medical inaccuracies this small piece of fiction highlights.
1. A medical student is not licensed healthcare provider. Therefore, they practice under someone else's license. They are managed by their attending physician or resident. They are not monitored by nursing. A nurse is not going to let a medical student do these things to her patient. The most a medical student does is obtain a patient history, do a physical exam, and observe procedures by other physicians. If this author had made the medical student a resident-- the scenario would be a little more plausible.
2. Every nurse is not that stupid. Sure, one nurse allowing a medical student to give her potassium I could believe. But, as in the novel, up to fifty? Remember, the nurse is likely more liable than the medical student under this circumstance. These nurses would all be fired. Nurses are not that blase about their licenses. Without one, even a license with a minor mark, and that nurse will not be working in nursing ever again. Medical students are learning. A nurse's job is to protect her patient. We don't trust medical students to be competent in what they're doing for that reason alone.
3. The author also misses another layer of protection. Medical dispensing machines are another layer of protection. Hospital medications are approved for dispensing by the hospital pharmacist. So, a pharmacist can look up a patient's lab results and check whether or not they need the potassium as well. All these medication orders on patients that don't need potassium is going to raise some serious alarms. Can you override the medication dispensing system? Yes, but you better have a good reason. Many hospitals have removed concentrated forms of IV potassium because an error could be so potentially deadly to the patient. Also, patients who receive a bolus dose of IV potassium need to be placed on an ECG tracing (or continuous heart monitoring.) In this instance, they are generally in the ICU or on telemetry and not a basic med/surg unit.
The scenario could be plausible if written another way. Overall, the author needed a seasoned ICU nurse to review the manuscript.
Labels:
Medical Students,
Medication Dispensing Machines,
Nurses,
Pharmacy,
potassium,
Scope of Practice
Tuesday, December 9, 2014
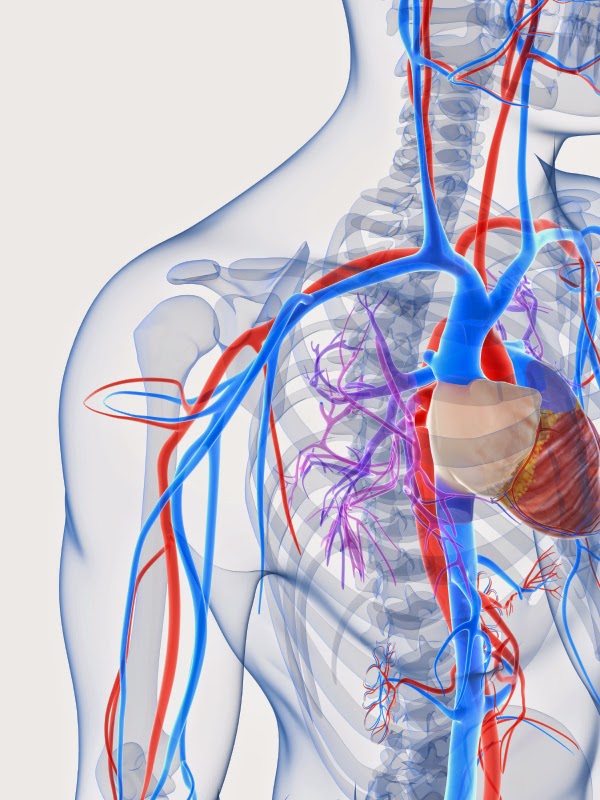
Author Beware: Use of Electricity
Authors, television producers and scriptwriters are fascinated by the use of electricity. This is probably one of the most commonly abused medical scenarios in that it is rarely used correctly.
One of my most popular posts here at Redwood's was a post titled Shock Me To Death that highlights how electricity (or defibrillation) should be used.
I was reading a debut novel by a medical doctor and found many grievous errors around the use of electricity. Which distresses me because he also said he had a cardiologist review the manuscript. Seriously, I kind of want to know who that doctor is and what kind of training he had.
There was the usual error of shocking a flatlined patient or asystole. Remember, in order for electricity to work, there has to be some present. If a patient is flatlined, there is no disorganized cardiac rhythm to reset and so defibrillation is contraindicated in those patient scenarios.
Next error in this manuscript was cracking the sternum down the middle during compressions. For one, the sternum is extremely hard to fracture. It's designed to protect some very important organs. If the sternum is even slightly fractured, we know there have been extreme forces placed on that patient. So, to have mere hands fracture a sternum all the way down the middle is ludicrous. Remember, they saw this open for open heart surgery. Breaking ribs is very probably during CPR, but not the whole length of your sternum . . . sorry.
Last, and most creatively (as I'd never seen this error before), was the amount of electricity used in an ICD device (an implanted cardiac defibrillator.) ICD's are devices that are used to convert patients from lethal arrhythmias like v-fib and v-tach. They are not pacemakers-- which stimulate the heart to beat.
Whenever electrodes are placed near the heart, the amount of electricity used is very small. Think about it. When we shock you from the outside of your body, the electrical current has a lot of tissue to pass through to get to your heart. This is why we use more. When defebrillating someone-- it's in joules.
A pacemaker uses a lot less energy. Outside pacemaker use milliamps.
And here is the very interesting quote from a published novel:
"Cardiologists shock patients all the time under controlled conditions, remotely dumping up to 700V (volts) of juice directly in to the heart via the ICD."
Wow. That's just . . . overkill.
Just how lethal is 700 volts applied directly to the heart?
This site explains that 110V can kill you.
It's so egregious an error that I'm not quite sure what this author was thinking. It pains me more that he is an actual medical doctor. I even double checked the published manuscript (as I'd read a galley proof before) and the error was still present.
I think he needs a new cardiologist.
One of my most popular posts here at Redwood's was a post titled Shock Me To Death that highlights how electricity (or defibrillation) should be used.
I was reading a debut novel by a medical doctor and found many grievous errors around the use of electricity. Which distresses me because he also said he had a cardiologist review the manuscript. Seriously, I kind of want to know who that doctor is and what kind of training he had.
There was the usual error of shocking a flatlined patient or asystole. Remember, in order for electricity to work, there has to be some present. If a patient is flatlined, there is no disorganized cardiac rhythm to reset and so defibrillation is contraindicated in those patient scenarios.
Next error in this manuscript was cracking the sternum down the middle during compressions. For one, the sternum is extremely hard to fracture. It's designed to protect some very important organs. If the sternum is even slightly fractured, we know there have been extreme forces placed on that patient. So, to have mere hands fracture a sternum all the way down the middle is ludicrous. Remember, they saw this open for open heart surgery. Breaking ribs is very probably during CPR, but not the whole length of your sternum . . . sorry.
Last, and most creatively (as I'd never seen this error before), was the amount of electricity used in an ICD device (an implanted cardiac defibrillator.) ICD's are devices that are used to convert patients from lethal arrhythmias like v-fib and v-tach. They are not pacemakers-- which stimulate the heart to beat.
Whenever electrodes are placed near the heart, the amount of electricity used is very small. Think about it. When we shock you from the outside of your body, the electrical current has a lot of tissue to pass through to get to your heart. This is why we use more. When defebrillating someone-- it's in joules.
A pacemaker uses a lot less energy. Outside pacemaker use milliamps.
And here is the very interesting quote from a published novel:
"Cardiologists shock patients all the time under controlled conditions, remotely dumping up to 700V (volts) of juice directly in to the heart via the ICD."
Wow. That's just . . . overkill.
Just how lethal is 700 volts applied directly to the heart?
This site explains that 110V can kill you.
It's so egregious an error that I'm not quite sure what this author was thinking. It pains me more that he is an actual medical doctor. I even double checked the published manuscript (as I'd read a galley proof before) and the error was still present.
I think he needs a new cardiologist.
Labels:
AED,
Asystole,
CPR,
Defibrillation,
Electricity,
Volts
Sunday, December 7, 2014
Up and Coming
Hello Redwood's Fans!
Are you enjoying the Christmas Season? How's the holiday shopping going?
I am excited to say that I am nearly done-- I'd give it a good 90% completion. I think this is going to be my goal in subsequent years. Shopping done in November. Presents wrapped by early December and then just enjoying the season.
For you this week!
An Author Beware series. These posts focus on what an author has done horribly wrong in a published novel. I never mention the book or the author (unless they are making millions and I know they can afford to hire me for medical consulting.)
This series focuses on two very common errors but this author used them in more egregious ways-- the use of electricity and scope of practice issues.
After that will be my annual blog break but I hope you'll tune in for the funny videos I share every year.
I hope each of you has a wonderful Christmas and exciting New Year. I'll be back to the medical mayhem on January 6th.
Much Love and Merry Christmas,
Jordyn
Thursday, December 4, 2014
Author Question: X-ray Anomalies
Barry Asks:
I have a character who is
getting X-rays for headaches and vision problems. The X- rays show some kind of
anomaly on or near the brain which requires a CT scan for further investigation.
The CT scan needs to show something. I said a shadow, but any anomaly would
work which cannot be biopsied due to the location.
For the development of the plot I need the doctors not to be able to ascertain immediately if the object on the scan is malignant or benign. Could this scenario work and would doctors wait to see what develops, or is there another course of action they would suggest in the absence of a biopsy?
For the development of the plot I need the doctors not to be able to ascertain immediately if the object on the scan is malignant or benign. Could this scenario work and would doctors wait to see what develops, or is there another course of action they would suggest in the absence of a biopsy?
Jordyn Says:
Very interesting question, Barry.
First of all, you're starting off with the wrong test. An x-ray (or plain film) is done merely to look at bones and is not the test indicated for your character's condition. A skull series would merely show fracture or bony tumors. It doesn't show brain tissue. Its primary indication is skull trauma-- looking for certain types of fractures that might indicate the need for neurosurgical evaluation.
What your character really needs, ultimately, is an MRI. This might solve both of your problems. The concern for a patient with headaches and vision problems is that they could have a brain tumor. An MRI has the ability, in some cases, to distinguish between malignant and benign tumors. So, if the tumor location is in an inoperable area, such as the pineal gland or corpus callosum, then you could build your scenario around this.
If, as the author, you want to have a wait and see period, then your option would be to have the tumor not be differentiated on MRI but small in size. Then, the doctors could do serial MRI's every 3-6 months to see if the anomaly changes.
However, the likely initial radiologic study of choice in the ER setting for your character's symptoms would be a CT scan of the head. The reason for this is that CT scans are very quick (less than five minutes.) An MRI of the brain can take anywhere from 30-60 minutes and are more expensive. What will show on CT is something bright white. Tumors and blood show up bright white on CT scan. Then, follow-up for the patient would likely be neurosurgical evaluation with an MRI scan.
The term "shadow" is more reserved for ultrasound studies according to the doctor I spoke with. So I would adjust your terminology in that aspect.
Best of luck with your novel!
Labels:
Brain Tumor,
CT scan,
MRI scan,
X-ray
Tuesday, December 2, 2014
What the Difference Between NICU and PICU?
Within the last several months, I was having a conversation with a reviewer and he interchanged the words NICU and PICU several times and it became clear to me that he didn't really understand the difference between these two units so I thought I would clarify that here today.
A NICU, aka Neonatal Intensive Care Unit, is specifically for babies who have just been born and are having difficulties. This includes premature babies (23-24 weeks is considered viable) up to normal gestational age of 40 weeks. This is their area of specialty.
The problem becomes-- when can the babies go back to the NICU if they become sick? Often times, a NICU won't take a premature baby back once they've been discharged home for a couple of months (even if they are still an infant) because they could be "contaminated" with all sorts of other-worldly germs. So, if the infant is sick enough and needs an ICU admission they will likely (though not always) be admitted to the PICU.
The PICU, aka Pediatric Intensive Care Unit, is for infants the NICU won't take and all other kids up to about the age of 18 (some up to 21) or whatever age the pediatric hospital has decided to admit. Even this age cut-off is becoming blurred because patients with chronic diseases (cystic fibrosis or special needs kids) might stick with their children's hospital well into their 20's. This is becoming an area of concern for pediatric institutions-- how to transition adults into adult-centered care.
Another way an adult might end up in the Pediatric ICU is if they have had a repaired congenital heart defect. There really is a limited number of adult cardiac surgeons who are comfortable operating on adults with these defects. In all honestly, it's only been in the last couple of decades that these kids were living to adulthood but improved surgical techniques have changed all of that.
A NICU, aka Neonatal Intensive Care Unit, is specifically for babies who have just been born and are having difficulties. This includes premature babies (23-24 weeks is considered viable) up to normal gestational age of 40 weeks. This is their area of specialty.
The problem becomes-- when can the babies go back to the NICU if they become sick? Often times, a NICU won't take a premature baby back once they've been discharged home for a couple of months (even if they are still an infant) because they could be "contaminated" with all sorts of other-worldly germs. So, if the infant is sick enough and needs an ICU admission they will likely (though not always) be admitted to the PICU.
The PICU, aka Pediatric Intensive Care Unit, is for infants the NICU won't take and all other kids up to about the age of 18 (some up to 21) or whatever age the pediatric hospital has decided to admit. Even this age cut-off is becoming blurred because patients with chronic diseases (cystic fibrosis or special needs kids) might stick with their children's hospital well into their 20's. This is becoming an area of concern for pediatric institutions-- how to transition adults into adult-centered care.
Another way an adult might end up in the Pediatric ICU is if they have had a repaired congenital heart defect. There really is a limited number of adult cardiac surgeons who are comfortable operating on adults with these defects. In all honestly, it's only been in the last couple of decades that these kids were living to adulthood but improved surgical techniques have changed all of that.
Labels:
Cardiac Surgery,
Congenital Heart Defect,
NICU,
PICU
Sunday, November 30, 2014
Up and Coming
Hello Redwood's Fans!
How was your Thanksgiving? Mine? Good. It was simple. My family and my parents. It was a joy to get to spend the day with them and not have to worry about going anywhere else.
Any Black Friday shoppers out there? Honestly, you will never see me get up early to go shopping. Even if offered a large sum of money. I. Don't. Do. Mornings. Plus, I really hate crowds and mall parking lots give me hives. This year I've done most of my shopping on-line.
We're back to the medical mayhem this week!
Tuesday: What is the difference between the NICU and PICU?
Thursday: Author question-- what's the best radiology study for a character experiencing headaches and blurred vision? Think you know the answer?
Have a great week and stay safe out there!!
Thursday, November 27, 2014
Happy Thanksgiving!
Hello Redwood's Fans!
A simple post, a simple smile, and a hope that your Thanksgiving is full of blessings and no medical mayhem.
Tuesday, November 25, 2014
Happy Thanksgiving Week!
Taking a short blog break this week for Thanksgiving celebrations. I know this time of year can be stressful because of the following cartoon. Most law enforcement officers and healthcare providers know that violence increases over the holidays because people come together who normally don't and there is alcohol and financial pressure on top of it.
That is a powder keg.
So, I'd like to offer the following suggestions if you're feeling like you'd rather take that carving knife to a family member rather than the turkey on the table.
1. Join the Polar Bears and take a swim in freezing water. This will definitely cool you off.
2. Volunteer to feed the homeless. This puts things in perspective.
3. Go to Alaska and feed the bears-- it's far away, stunning scenery and you'll be so thankful if you live through the experience.
If those aren't an option-- watch a funny video and remember-- it's only a day. Or a few days.
Most importantly-- don't do anything that will land you in jail.
Blessings, Jordyn
P.S.-- There is some mild language in this video. You've been forewarned.
Thursday, November 20, 2014
Author Beware: Arteries vs. Veins
Do any of you watch the chef Gordon Ramsey? He's a well-known British chef with a serious temper. It's been well displayed on many of his shows. At times, he just begins to bang his head on the counter at the incompetence of some of his chefs.
That's how I felt when I read this sentence in a manuscript.
"Her vein began to throb at her temple."
Perhaps, I shouldn't be so harsh. This person doesn't have a medical background and perhaps it isn't common knowledge that there is a big difference between arteries and veins.
There is.
Arteries carry blood away from your heart where it has just been oxygenated by your lungs. In order to carry the blood forward, the heart beats to propel it. Therefore, when an artery is severed, the blood spurts out with each heart beat in a fairly dramatic fashion. There is no question from the medical staff-- "Do you think he got an artery?" It more like, "We've got a bleeder!" The blood is a brighter red because it is loaded with oxygen.
Only arteries throb. That's how we feel your pulse-- at an artery.
Veins carry blood to your heart to get reoxygenated. They don't pulsate. The blood is darker in color and tends to ooze though if enough veins are severed-- the bleeding can be quite brisk.
The correct way to phrase the above sentence would have been:
"The artery at her temple began to throb."
And remember, all bleeding can lead to death if not controlled-- whether is be venous or arterial.
Tuesday, November 18, 2014
On the Fringe Of Medicine: Braxton DeGarmo, MD
Have you ever watched a TV show or movie, or
finished a novel, and found yourself scratching your head at the end, wondering
how that writer came up with such a lame idea? If the story was a medically or
technology based one, there’s a good chance the writer was flirting with the
edge of good science – not cutting-edge or state-of-the-art, but
pseudo-science, fringe medicine, or, as some call it, deviant science – and
fell off.
Now, I’m not talking about badly portrayed medicine.
Television is full of that. I don’t think a week goes by without some character
getting an injection into the neck or just above the elbow, neither of which is
medically valid. Or what about those lead characters who get shot in the chest,
just below the shoulder, and are back at work, busting the bad guys in a week,
or less? Trust me, if you’re a writer, don’t use TV, or the movies, as your
source of research. I’m sure you already know that.
I am talking about the actual science or medicine
behind a story. Is it reality or something on the fringe of science? In
medicine, that fringe is often called “alternative” medicine. Such practices as
homeopathy and radionics (psionics or dowsing) fall into the “alternative”
category, as does aromatherapy, the use of oils, much of herbal medicine, psychic
healing, iridology, reflexology, cupping, and more. To date, these forms of therapy
have not been scientifically proven and rely on anecdotal accounts of their
benefits alone. Each subjective testimony is fraught with potential bias and
error, and double-blind testing of such claims has typically failed to show any
advantage. You never hear of the treatment failures, just the stories of those
claiming positive results.
Please note that, in this post, I’m excluding
“neo-traditional,” or ethno-medicine, which consists of traditional,
culturally-based forms of treatment such as acupuncture. While these therapies
cannot be explained scientifically, some of them have been shown to work and
studies into why they work are on-going.
If you decide to include some form of “alternative”
medicine in your story, don’t be surprised to find them explained in technical,
scientific terms when you research them. Herbal medicine has renamed itself
“naturopathy.” Radionics has its mysterious “black box” that looks like a
scientific instrument. One of the trends in “alternative” medicine is to take
on scientific trappings to make the modality seem legit and of proven benefit.
Mentioning a character’s use of one of these
therapies as simply one more layer of her personality is unlikely to cause you
problems. However, the risks of using “alternative” medicine in any significant
way in a story are many. You must present it accurately, not just in scientific
terms, but as its proponents present it. Even when you do so, you run the risk
of alienating readers on both sides of that fence. Disbelieving readers might
be turned off by its use, while advocates might get angry if it’s used
negatively or presented as fraudulent.
And that gets to the crux of using fringe medicine,
or science in general, in our writing. If it’s to be a major part of the story,
you must make the idea believable. You, the writer, must get the reader to
suspend his or her beliefs long enough to accept the premise. The further out
on the fringe that therapy is, the harder that task becomes.
*****************************************************************
*****************************************************************
Braxton DeGarmo, MD is a retired Emergency Medicine
physician who lives outside St. Louis, MO with his wife and garden. He is the
author of cutting-edge Christian fiction, whose titles include: The MilitantGenome, Indebted, Looks that Deceive, Rescued and Remembered, and The Silenced Shooter. You can learn more
about him at www.braxtondegarmo.com,
or on Facebook at www.facebook.com/Braxton.DeGarmo.Author.
He also tweets from @braxtondegarmo.
Sunday, November 16, 2014
Up and Coming
Hello Redwood's Fans!
How has your fall been treating you? Anyone out there trying all the new pumpkin spiced products? Me . . . of course! Here's the rundown on what I've tried. Pumpkin Spice Oreo cookies. These were okay. I don't know that I would seek them out. Pumpkin spiced whipped peanut butter. Yes, you read that right. This was enjoyable but not sweet enough for me. Then there are the pumpkin spiced and pumpkin cheesecake donuts from Krispy Kreme.
So . . . the winner is . . . the pumpkin cheesecake donuts from Krispy Kreme!! They are yummy. And, I would like to publicly thank the woman who gave me the LAST pumpkin spiced donut of the day to try. I'd waited three weeks to stop by the store so you totally made my day!
What pumpkin spiced treat are you enjoying?
For you this week . . .
Tuesday: Author and ER physician Braxton DeGarmo stops by to discuss "fringe" medicine. Exactly what that is and what it means.
Thursday: Fellow writers . . . please . . . this is becoming very problematic. An author beware post on the difference between arteries and veins.
Have a great week!!
How has your fall been treating you? Anyone out there trying all the new pumpkin spiced products? Me . . . of course! Here's the rundown on what I've tried. Pumpkin Spice Oreo cookies. These were okay. I don't know that I would seek them out. Pumpkin spiced whipped peanut butter. Yes, you read that right. This was enjoyable but not sweet enough for me. Then there are the pumpkin spiced and pumpkin cheesecake donuts from Krispy Kreme.
So . . . the winner is . . . the pumpkin cheesecake donuts from Krispy Kreme!! They are yummy. And, I would like to publicly thank the woman who gave me the LAST pumpkin spiced donut of the day to try. I'd waited three weeks to stop by the store so you totally made my day!
What pumpkin spiced treat are you enjoying?
For you this week . . .
Tuesday: Author and ER physician Braxton DeGarmo stops by to discuss "fringe" medicine. Exactly what that is and what it means.
Thursday: Fellow writers . . . please . . . this is becoming very problematic. An author beware post on the difference between arteries and veins.
Have a great week!!
Thursday, November 13, 2014
Dissociative Identity Disorder: Part 2/2
Today, author Robin E. Mason concludes her two part series on Dissociative Identity Disorder. You can find Part I here.
The problem with DID is
identifying it. Patients often live with DID for several years before they seek
treatment. Even then, they may go through an extensive process of elimination
before it is properly and correctly identified. The difficulty lies in that its
symptoms are parallel to other mental and emotional disorders, and include:
- Depression, suicidal tendencies
- Mood swings
- Flashbacks, memory problems, selective loss of memory
- Insomnia, night terrors, sleep walking
- Anxiety, panic attacks, phobias
- Alchohol and drug abuse – it is interesting to note that DID is not cause by substance abuse, but may, in fact, trigger it.
- Disorientation and confusion
- Compulsions and rituals – OCD behavior
- Auditory and visual hallucinations
- Eating disorders
Perhaps the hallmark symptom of
DID is its fugue states: periods of time, from minutes to days, in which an
individual has no memory of events, or of time itself. Different personalities, or alters, will surface
in specific circumstances. Each alter splinters off for that purpose, to cope
with various life events. The consensus theory on the cause of DID is extreme
childhood trauma, usually associated with sexual abuse. Triggers can be a
visual setting, a voice, photo, food – any stimuli that brings unwanted
memories to surface. It is at this point an alter steps in to cover for the host or primary personality. Typically
the host has no memory of what his or her alter does. Alter personalities,
however, mostly are aware of other alters and their actions.
Treatment for DID is found
through long-term psychotherapy, hypnotherapy, and/or art, music or movement
therapies. The objective, of course, is to integrate the alters into a singular
and whole – multidimensional - person. As DID is not physiologically induced, there
is no medication to treat it. However, accompanying disorders like depression
or anxiety may be treated with medication and thus alleviate some of the DID
symptoms or triggers.
There is some school of thought
that DID is not legitimate, but is iatrogenic, or that it is created by
suggestion of the therapist. However, brain imaging studies have provided
evidence of physiological changes in some patients.
As for Sybil, some question arose
at the authenticity of her diagnosis. Dr. Wilbur was accused of falsifying her
findings. At one point, Sybil, whose real name was Shirley Mason, admitted to
making the whole thing up. She later recanted that admission.
It seems to me that whatever Dr.
Wilbur’s motivations were, Sybil’s story was not entirely untrue If, on one
extreme, the whole thing was the wild creation of her and Dr. Wilbur, that
speaks of something horribly wrong – which would then be another issue and
sickness. We will never know if what happened in her childhood triggered panic
attacks and black-outs. I believe there was truth in her story, 10% or 100%, I
can’t say. I believe it stirred an interest in the condition, and in turn
childhood abuse.
Previously,
I said I learned why Sybil’s story intrigued me. Not because of sexual
molestation, because I wasn’t. And not because I ever suffered DID, because I
haven’t. But something about her dark childhood rang true with me, however
different that might have been. I felt that I was in a dark hole, unwanted,
unwelcome, and unloved. In that, I can identify with Sybil. And in that, my
fascination with DID and crises of identity. I know now, too, that I am whole,
I am wanted, and I am loved.
******************************************************************************
******************************************************************************
Robin Mason lives in upstate South Carolina where
she began writing as self-proscribed therapy in 1995. Life threw a few
(dozen) (thousand) hiccups and curve balls, and she got serious about working
on her debut novel, Tessa,
in 2013. Robin’s greatest priority and highest calling is to honor God in all
she does, especially with the talents and abilities He’s given her. Like
writing.
Tuesday, November 11, 2014
Dissociative Identity Disorder: Part 1/2
I'm pleased to host author Robin E. Mason on Redwood's Medical Edge who will be guest blogging in two parts on Dissociative Identity Disorder AKA Multiple Personality Disorder.
Welcome, Robin!
I was first intrigued with this phenomenon, then called Multiple Personality Disorder, when the movie Sybil starring Sally Field came out in 1976. At the time, I couldn’t have said what about it so intrigued me. I would only learn the reason years later.
As with any phenomenon, I believe there is nothing new under the sun, only our awareness of it. Sure, epidemic waves run their course, and then there may be little or no action for a time and then – BAM it strikes again.
The National Alliance on Mental
Illness defines Dissociative Identity Disorder (DID) as involving a disturbance of identity in which two or more separate and
distinct personality states (or identities) control an individual’s behavior at
different times. They further state that each identity, or alter, may exhibit differences in speech,
mannerisms, attitudes, thoughts and gender orientation… even present physical
differences, such as allergies, right-or-left handedness or the need for
eyeglass prescriptions. Psychology
Today states it this way, failure to
integrate various aspects of identity, memory and consciousness in a single
multidimensional self.
We all have different and varying
roles in our lives – multidimensional selves - and we continually switch back
and forth. The difference is, I am fully aware when I am being my writer-self –
like right now – and when I must (force myself to) be my homemaker-self, i.e.
vacuum and do the dishes. I delight in my granny role, and fully enjoy
activities with my granddaughters. Still, all is done fully aware of my
different roles, and all are done with the same basic personality traits. I
have more fun with it that perhaps most people, though, because I am also an
actress, and will switch accents on a whim. Yeah, I do that!
Double consciousness, or dédoublement, the historical precursor
to DID surfaced in the 19th century, which was observed as sleepwalking. Hypotheses
claimed this to be switching between a
normal consciousness and a somnambulistic state. (Wikipedia)
Come back Thursday for Part II.
**********************************************************************
Robin Mason lives in
upstate South Carolina where she began writing as self-proscribed therapy in
1995. Life threw a few (dozen)
(thousand) hiccups and curve balls, and she got serious about working on her
debut novel, Tessa,
in 2013. Robin’s greatest priority and highest calling is to honor God
in all she does, especially with the talents and abilities He’s given her. Like
writing.
Labels:
Dissociative Fugue,
Dissociative Identity Disorder,
Multiple Personality Disorder,
Robin E. Mason
Sunday, November 9, 2014
Up and Coming
Hello Redwood's Fans!
How has your week been?
Mine-- getting back into the swing of life. The holidays are upon us and I'm seriously going to get my Christmas shopping done early this year. I mean, everything wrapped and under the tree by December 1st.
Don't hate me.
I'm usually not so far ahead of things but I find that once these are done-- I can focus just on friends, family and Christ.
This week, friend and author Robin E. Mason is stopping by to talk about Dissociative Identity Disorder. She presents some really interesting information and I hope you'll check out her new novel, Tessa.
Have a great week!
How has your week been?
Mine-- getting back into the swing of life. The holidays are upon us and I'm seriously going to get my Christmas shopping done early this year. I mean, everything wrapped and under the tree by December 1st.
Don't hate me.
I'm usually not so far ahead of things but I find that once these are done-- I can focus just on friends, family and Christ.
This week, friend and author Robin E. Mason is stopping by to talk about Dissociative Identity Disorder. She presents some really interesting information and I hope you'll check out her new novel, Tessa.
Have a great week!
Thursday, November 6, 2014
Right to Die: Should It Be Legal?
Recently, two cases involving the "right to
die" have been in the news. One more so than the other.
The first is the case of twenty-nine-year-old Brittany
Maynard. Sadly, Brittany was diagnosed with an aggressive form of brain
cancer. She attempted surgery which did remove most of the tumor but it grew
back in a period of two months. At that point, she declined further treatment,
to live her last days to the fullest.With one caveat. She wanted to choose the method and time of her death.
Her family intentionally moved to Oregon which in 1997 enacted the Death with Dignity Act which allows physicians to prescribe lethal medications expressly for the purpose of ending one's life.
Which she did on November 1, 2014.
The second case is of Nancy Fitzmaurice, age 12, whose mother petitioned the court in the UK and won the right to let her daughter die by withdrawing food and fluids. It took 14 days. Sometimes I have trouble knowing for sure if things reported in England papers are true because I don't know what reliable sources are "over the pond" so take this with a grain of salt. I researched Snopes and didn't find it listed there as false.
Here is my take.
Case One:
Though sad, Brittany is an adult with a diagnosed terminal condition. Though I think every moment of life is precious and wouldn't choose this for myself, I support her right as an adult to do this. I think the right to die should be severely limited to cases like Brittany's and not be used for things like depression, mental illness and most chronic conditions. I'm not an expert on the Oregon law but I think two independent physicians should certify that the patient does have a terminal condition that will lead to death.
Case Two:
This case, if true, I am wholly against. First of all, food and water is a basic need. Allowing her to die by withdrawing food and fluid was torture. I'm sorry but it's true. You can't even do that to an animal without being put in jail. But-- is that the only way it's "appetizing" to the public? Honestly, actively taking her life would have been more humane. I think if this family could not emotionally, physically, or financially take care of her anymore than other alternatives should have been considered. She was a minor. She was disabled. These are who we are called to care for.
What say you?
The second case is of Nancy Fitzmaurice, age 12, whose mother petitioned the court in the UK and won the right to let her daughter die by withdrawing food and fluids. It took 14 days. Sometimes I have trouble knowing for sure if things reported in England papers are true because I don't know what reliable sources are "over the pond" so take this with a grain of salt. I researched Snopes and didn't find it listed there as false.
Here is my take.
Case One:
Though sad, Brittany is an adult with a diagnosed terminal condition. Though I think every moment of life is precious and wouldn't choose this for myself, I support her right as an adult to do this. I think the right to die should be severely limited to cases like Brittany's and not be used for things like depression, mental illness and most chronic conditions. I'm not an expert on the Oregon law but I think two independent physicians should certify that the patient does have a terminal condition that will lead to death.
Case Two:
This case, if true, I am wholly against. First of all, food and water is a basic need. Allowing her to die by withdrawing food and fluid was torture. I'm sorry but it's true. You can't even do that to an animal without being put in jail. But-- is that the only way it's "appetizing" to the public? Honestly, actively taking her life would have been more humane. I think if this family could not emotionally, physically, or financially take care of her anymore than other alternatives should have been considered. She was a minor. She was disabled. These are who we are called to care for.
What say you?
Tuesday, November 4, 2014
Ebola: Is it Airborne?
I'm just not convinced it can be wholly said that there should be no concern that Ebola cannot be transmitted through the air.
Even if Ebola Zaire, which is the strain responsible for the current outbreak in West Africa (and is also the most virulent with up to a 90% kill rate) is not airborne-- I'd like to highlight the discovery of Ebola Reston as thoroughly discussed in Richard Preston's nonfiction title The Hot Zone which presents case studies of four Ebola viruses (Marburg, Ebola Sudan, Ebola Zaire and Ebola Reston.) It is a must read.
Even if Ebola Zaire, which is the strain responsible for the current outbreak in West Africa (and is also the most virulent with up to a 90% kill rate) is not airborne-- I'd like to highlight the discovery of Ebola Reston as thoroughly discussed in Richard Preston's nonfiction title The Hot Zone which presents case studies of four Ebola viruses (Marburg, Ebola Sudan, Ebola Zaire and Ebola Reston.) It is a must read.
First of all, these viruses are relatively new. They first showed up in the 1970's literally out of nowhere. Why do I say that? Because the reservoir for these viruses has never been found. No one knows where it comes from or what plant, insect, or animal it might live in without killing it. It is thought that Kitum Cave in Mount Elgon National Park is a likely candidate but testing of several species within the cave haven't found the host.
Ebola is a filovirus or thread virus. It has a distinctive look under microscope resembling a jumbled mass of tangled threads with eyelets or shepherd's hooks on the end. There are currently five species of Ebola virus: Zaire, Bundibugyo, Sudan, Reston and Tai Forest. All have varying degrees of virulence.
To learn how Ebola kills-- check out this video.
To learn how Ebola kills-- check out this video.
Let's get back to Ebola Reston. This strain of Ebola was first discovered in a monkey house in Reston, VA in 1989. This facility housed monkeys from overseas for several months to prove they were healthy before being sold to research facilities.
There were several different rooms to this monkey house but the facility did share one ventilation system. An illness began to break out among the monkeys that killed them swiftly. The animals would lose their appetite, develop a mask-like quality to their face, become inactive and die within one to two days. At times, they had bleeding from their noses. Necropsy done by an employee of the facility showed large, hardened spleens and evidence of internal bleeding.
This employee decided to send samples to the United States Army Medical Research Institute of Infectious Diseases (USAMRIID) which was nearby and after testing over days and weeks-- it was discovered that this was a new strain of Ebola. At that particular time, only Ebola Sudan and Ebola Zaire were known.
The interesting thing about Ebola Reston is that it is airborne. It traveled through that monkey house, room to room, and began killing animals that hadn't had any direct contact with one another. It was so concerning to the Army because of the facility's location to Washington D.C. that a decision was made to "nuke" the entire animal population and gas the building to kill every microscopic living thing inside. This led to hundreds of animals being euthanized.
Then, it happened again. More animals were brought in from overseas and the virus went loose. Likely, the animals brought it with them and it was not present in the facility.
On autopsy of these monkeys, it can be seen that the virus was located in their lungs-- ready to burst from air sacs. This is how airborne transmission works. The virus is coughed up and expelled into the air where another person breathes it in.
When the second incident of Ebola Reston hit the monkey house-- they let it run its "natural course" since they had also discovered it didn't cause illness in humans. When they did that-- 100% of the monkeys died.
What's interesting about the Reston, VA monkey house workers was that they all seroconverted from the illness. This means they were infected, their body built up antibodies, but they didn't get sick. What's scary is that genetically speaking-- researchers don't really know what makes Ebola Reston all that different from Ebola Zaire. The question becomes . . . how easy would it be for these other Ebola viruses that do cause serious illness in humans to change one protein structure to then be airborne like Ebola Reston?
The answer is . . . they don't know. What they do call Ebola in general-- a slate wiper. People who know a lot about Ebola lose sleep over this virus.
Personally, as a healthcare provider, I think it's safest to operate under the assumption that it has the potential for airborne spread. We should be using the same level of protection when working with this virus that the US Army does-- which they classify as a Level 4 Hot Agent. You wear a space suit working with these pathogens. People who work with Level 4 Agents are viewed as a little crazy according to Preston's book.
I don't think we respect this virus enough. Here in the US-- people are very blase about its potential to kill. Keep in mind that those that survived here were treated early by a highly specialized medical system and received experimental treatments that likely helped them fight off the virus.
Would you consider this adequate?
Labels:
Ebola,
Ebola in the USA,
Ebola Reston,
Ebola Virus,
Ebola Zaire
Monday, November 3, 2014
Up and Coming
Hello Redwood's Fans!
What an interesting week it has been-- medically speaking. Lots of medical things in the news. I tried to tune it all out while I was on my writing retreat (of which, I did get a lot of writing done!) but quickly was inundated with medical stories upon my return and my inner medical nerd couldn't help but start doing more research.
Plus, I had to go to my hospital for mandatory Ebola training-- like two days after my lake retreat. It's hard to go from the first photo to the second photo. Reality can hit hard sometimes.
This week, I'm focusing on some of these interesting medical cases that could easily be worked into a fiction novel.
Tuesday: Can we say for sure Ebola is not airborne? I'll give you my take tomorrow.
Thursday: The Right to Die? Should it be allowed? If so, under what circumstances?
Have a great week.
Thursday, October 30, 2014
Injuries Related to Mass Casualty Incidents: Blast Lung Injury
Bombings are becoming not so rare an incident in today's society. If you decide to write a novel surrounding a mass casualty incident related to a bombing-- consider using this injury: Blast Lung.
Blast Lung is the most common fatal injury related to bombings. It's reported to be more common in patients with skull fracture, >10% burns and impaled trauma to the head/chest.
A patient can present with some of the following diagnoses as well that fall under this umbrella of injury:
- Bruise to the lung (Pulmonary Contusion).
- Blood or air in the chest cavity (Hemo/Pneumothorax).
- Traumatic Emphysema (tight lungs with poor oxygen exchange).
Blast lung should be suspected if the patient presents with difficulty breathing, shortness of breath, cough, coughing up blood, chest pain and low oxygen levels. On chest x-ray a distinctive butterfly pattern can be seen.
Treatment is supportive in nature. Oxygen, giving fluid to prevent shock but not too much as to overload the lungs, and a ventilator if the patient is in impending respiratory distress/failure.
To read more about mass casualty incidents check out the following link:
Mass Casualty Incident: An Overview
Labels:
Blast Lung Injury,
Mass Casualty Incidents
Tuesday, October 28, 2014
Injuries Related to Mass Casualty Incidents: Mucormycosis
Sometimes, as an author, you need something unusual to inflict your character with so this week I thought I'd focus on two injuries that can be unique to mass casualty incidents.
Mass casualty incidents (MCI's) are defined as those that overwhelm equipment and personnel by the number casualties. It's not necessarily the same for every organization. If a rural EMS crew comes upon a three-car accident with three patients-- that might be a mass casualty incident for them but this same accident happening in downtown New York would not be.
Often times, when we think of mass casualty incidents, we recall the big things like tornadoes, earthquakes and terrorist attacks (bombings, nerve gas release) and school shootings.
For this post I'm focusing on a unique infection related to Acts of God weather events and next post I'll do an injury related to bombings.
Mucormycosis is a soil fungus that comes out to play when it is dredged up from the earth with events like flooding and tornadoes. Usually a person comes into contact with the fungus via an impaled object. It is a necrotizing bug (meaning is devours flesh) so aggressive debridement and treatment with broad spectrum antibiotics and antifungals is necessary.
After the Joplin, MO tornado in 2011-- thirteen cases were identified of which five (38%) died. Most had accompanying fractures. Interesting to note is that all the patients were located in the zone that sustained the most damage. Infection was associated with penetrating trauma and multiple wounds. You can read further about this rare infection by reading this piece as well.
What also could have contributed to the number of infections was the devastation to the medical system that happened during the tornado as well. The main hospital was damaged and several off-site clinics were set-up so the above news piece surmises that wounds may not have been adequately treated (which would be serious irrigation.) This is understandable considering what the town was dealing with.
What about you? Have you ever been in a natural disaster?
Labels:
Fungal Infection,
Fungus,
Mass Casualty Incidents,
Mucormycosis Infection,
Natural Disasters,
Necrotizing Fasciitis
Sunday, October 26, 2014
Up and Coming
Hello Redwood's Fans!
How has your week been? Mine? Hopefully fabulous as I'm out of town enjoying a writer's retreat. My first one ever. I'll give you a full report upon my return.
Hopefully, you've taken advantage of the fire sale on my novels (Proof, Poison and Peril.) We're in the last few days of this promotion so no more waiting!
This week I'm dealing with injuries related to mass casualty events. As you know, mass casualty events (whether Acts of God or terrorist events) can quickly overrun the medical system. Not only are we dealing with a large number of patients, but there may be new injuries that we're not used to dealing with as well.
Tuesday: Mucormycosis infection. Just what is it and when should you worry about it?
Thursday: Blast lung. This is related to bombing events.
Hope you have a great week and have a safe Halloween!
How has your week been? Mine? Hopefully fabulous as I'm out of town enjoying a writer's retreat. My first one ever. I'll give you a full report upon my return.
Hopefully, you've taken advantage of the fire sale on my novels (Proof, Poison and Peril.) We're in the last few days of this promotion so no more waiting!
This week I'm dealing with injuries related to mass casualty events. As you know, mass casualty events (whether Acts of God or terrorist events) can quickly overrun the medical system. Not only are we dealing with a large number of patients, but there may be new injuries that we're not used to dealing with as well.
Tuesday: Mucormycosis infection. Just what is it and when should you worry about it?
Thursday: Blast lung. This is related to bombing events.
Hope you have a great week and have a safe Halloween!
Thursday, October 23, 2014
Author Question: Suicide Attempts That Could Lead to Brain Death
Jennifer asks:
I am trying to find a scenario where a suicide attempt would
lead to traumatic brain injury with long-term repercussions (reduced mental and
physical functioning afterward) but not death.
Jordyn says:
There are
actually several ways a person could attempt suicide and end up with a brain
injury. It doesn't have to be a traumatic brain injury but anything that would
lead the person to have a hypoxic event (where they weren't breathing for a
period of time) could lead to brain damage and difficulty down the road.
If you want direct brain injury then
a gunshot wound to the head would be the best bet. Maybe it was misdirected
somehow and the person just got a glancing blow.
If you want to go with the lack of
oxygen aspect then:
1. Attempted hanging.
2. Drug Ingestion.3. Ingestion of poison.
4. Cutting the wrists-- if you lose enough blood you will code which could lead to an hypoxic event as well.
Really, any suicide attempt that leads to a code event can cause
brain injury.
Follow-up question . . .
Follow-up question . . .
Jennifer asks: Would it be covered by insurance since it was a self-inflicted injury?
Jordyn says: Medical insurance will cover if it is a self-inflicted injury. You might be thinking of life insurance that usually does have a clause where if a person dies as a result of suicide the life insurance policy won't pay out. However, from my personal experience with purchasing life insurance policies, this is usually limited to the first 6 months to two years of the policy depending on the insurer.
*************************************************************************
Jennifer Slattery writes missional romance novels for New Hope Publishers and Christian living articles for Crosswalk.com. You can visit her online at http://jenniferslatterylivesoutloud.com/
Tuesday, October 21, 2014
Author Question: Death by Bee Sting
Amie Asks:
My character is allergic to bees. The villains plan
on using bee venom to make her death look like an accident if they need to. Is
there any drug that would mimic bee venom, or will I need to use actual bees?
Jordyn Says:
There is no drug that I'm aware of that would mimic bee venom so I think you're going to need to use the real thing. You could just have the killer trap a bee against her body so it actually stings her versus trying to gather bee venom and try to inject her with it.
What actually kills a person if they are allergic to bees is not the bee venom itself-- it's the body's response to the bee venom and the response it mounts is called anaphylaxis.
I think I should point out the difference between an allergic reaction and anaphylaxis. An allergic reaction is a localized response (I get stung by a bee and my whole arm swells up) or a skin rash.
Anaphylaxis is a multi-system reaction due to massive histamine release that leads to capillary leaking, massive swelling and edema. Anaphylaxis is defined as having two or more body systems involved reacting to the substance and can be two or more of the following.
Skin: Hives.
Gastrointestinal: Vomiting or diarrhea.
Respiratory: This would include anything from the mouth to the lungs. Lip swelling. Tongue is swelling. Itchy, scratchy throat. Thick feeling to the throat. Difficulty swallowing. Drooling. Wheezing in the lungs. Low oxygen levels.
Cardiovascular: Increased heart rate and low blood pressure.
When we treat anaphylaxis-- each treatment is designed to stop the reaction. The more body systems involved, the more life threatening the reaction is.
#1 Drug given: Epinephrine via an intramuscular injection. Why not IV? An IV dose in a conscious person could cause enough coronary artery vasoconstriction to give the person a heart attack.
#2 Drug: Inhaled Albuterol IF the person is wheezing.
#3 Drug: A Steroid. If the person has multiple system involvement (particularly respiratory or cardiovascular) then this will be given IV. If not, then an oral dose is okay.
#4 Drug: Benadryl or diphenhydramine. This blocks one form of the histamine being release (H1 blocker). IV if sick, otherwise by mouth.
#5 Drug: An antacid like Zantac or Pepcid. This blocks the other form of histamine being released (H2 blocker). And same here, too-- IV if sick, otherwise orally.
Patients with anaphylaxis are monitored for 8-12 hours after medications are given. Patients who require more than one dose of IM epi may be admitted to the hospital. The reason is that when the medication wears off we want to ensure the reaction doesn't come back. Patients will go home with a script for an Epi Pen (or renewal script), a steroid for three days and then H2 blocker for three days.
If you're interested in more information-- here is a post I did on food allergies.
Labels:
allergic reaction,
anaphylaxis,
Bee Sting,
Emergency Care for Anaphylaxis,
Treatment for Allergic Reaction,
Treatment for Anaphylaxis
Sunday, October 19, 2014
Up and Coming
Hello Redwood's Fans!
Ready for Halloween and all the spooky movies about to release? Or, would you rather read great books instead?
If it's books-- then I have good news for you. The e-books of my entire trilogy (Proof, Poison and Peril) are going on sale this coming week! I hope you'll take advantage of it-- particularly the first few days when each title is a mere $0.99!!
For you this week . . .
Tuesday: Death by bee sting. Is it possible? Is there a drug that could mimic this?
Thursday: What types of suicide attempts can lead to a traumatic brain injury?
Have a great week!
Ready for Halloween and all the spooky movies about to release? Or, would you rather read great books instead?
If it's books-- then I have good news for you. The e-books of my entire trilogy (Proof, Poison and Peril) are going on sale this coming week! I hope you'll take advantage of it-- particularly the first few days when each title is a mere $0.99!!
For you this week . . .
Tuesday: Death by bee sting. Is it possible? Is there a drug that could mimic this?
Thursday: What types of suicide attempts can lead to a traumatic brain injury?
Have a great week!
Thursday, October 16, 2014
Parents Behaving Badly: The Case of Justin Ross Harris
As a pediatric nurse, I've been intrigued by the case of Justin Ross Harris, who is accused of killing his son by leaving him in a hot car.
This is one of those things, personally, that I do kind of scratch my head at. I know people get stressed. I could even understand leaving a child behind for a few moments before your rationale brain kicked in and said, "Hey, the baby's in the car."
I mean, we treat phones so much better.
He has pled innocent but this CNN HLN article brings up some interesting points that came from his hearing that I thought I would highlight here. These come directly from their piece.
1. It was a normal morning. Meaning, he was the one who usually took his kid to school. It wan't unusual for them to stop at Chik-fil-A for breakfast. When you do things repeatedly, there's less room for error.
2. It's a short distance from Chik-fil-A to his daycare. Like one minute. So, in one minute, he loaded his son up in the car but then forgot he was there.
3. You could see the child from the rear view mirror. This is a pretty interesting point. Evidently, Harris backed into his parking spot. He doesn't have a rear view camera so would have had to look in his mirror. When they placed a mannequin of similar size in that seat it was visible in the mirror.
4. Bizarre behavior. Witnesses felt like he was "working" at being emotional.
5. Strange statements. One alleged statement: "I dreaded how he would look."
6. Additional Injuries. Abrasions to the back of the head.
7. Sexting. Harris was sexting six different women as his son died including sending explicit photos.
8. Life Insurance. The child had two life insurance policies on their son and might have been in financial trouble from credit card use.
9. Internet Activity. Disturbing internet searches for videos with people dying, how to be child-free, how to survive prison and the age of consent for Georgia.
10. Harris is deaf in his right ear. This is used by the defense to perhaps explain that he didn't hear his son in the car.
Whatever happens in this case, one good thing that might come from these deaths is the invention from one teen, designed to alert parents if they do accidentally leave their child in the car.
What do you think from what you've hear of the Harris case? Do you think he committed murder?
Labels:
Child Abuse,
Child Left In Hot Car,
homicide,
Hot Car Deaths,
Murder
Subscribe to:
Posts (Atom)